When you work in nutrition care, clear, precise language isn’t optional—it’s essential. Enter the world of nutrition diagnosis terminology: the standardized vocabulary used by dietitians and allied health professionals to define, communicate and address nutrition-related problems.
At its simplest, a nutrition diagnosis is a concise statement of a nutrition problem the practitioner can address. But why does it matter that we use a standardized terminology for it? Because without shared language, we risk miscommunication, inconsistent documentation, and ultimately, weaker outcomes for clients and patients.
Using the same terminology helps everyone—from the dietitian writing the note to the physician reviewing the care plan to the electronic health record system—to understand exactly what is meant. This is why terminology becomes a bridge for care and continuity, especially in interprofessional teams and complex healthcare settings.
The Nutrition Care Process (NCP) Framework
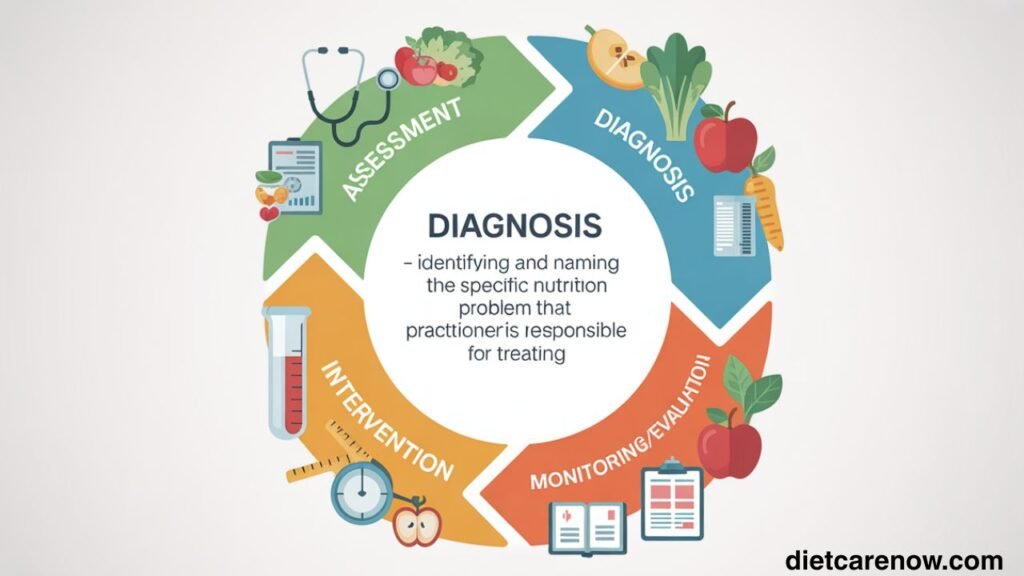
Let’s ground the discussion in the broader framework that drives nutrition practice: the Nutrition Care Process (NCP). The NCP is a systematic, four-step model used by credentialed nutrition and dietetics professionals to deliver safe, effective, and quality nutrition care.
The four main steps are:
- Assessment – gathering data about the client’s nutrition-related and health status.
- Diagnosis – identifying and naming the specific nutrition problem that the practitioner is responsible for treating.
- Intervention – planning and implementing actions to address the nutrition diagnosis.
- Monitoring/Evaluation – tracking client progress, reassessing, and adjusting the plan as needed.
Understanding how nutrition diagnosis terminology fits in: it is central to Step 2 (Diagnosis). But it also influences how we write the intervention (Step 3) and how we measure outcomes (Step 4). Without clear diagnosis terms, the rest of the process can become fuzzy.
Also read: /tuna-salad-shelf-life/
Understanding Nutrition Diagnosis
What is a nutrition diagnosis?
In the simplest terms: it’s a nutrition problem that has been identified during assessment and for which you (as a dietitian or nutrition professional) are responsible and capable of intervening.
How does it differ from a medical diagnosis?
A medical diagnosis defines a disease or health condition (for example: type 2 diabetes, chronic kidney disease, congestive heart failure). A nutrition diagnosis is distinct: it describes a problem related to nutrition—intake, clinical, behavioral, environmental—that can be addressed by dietetics care. The key difference: the scope of intervention. The nutrition diagnosis is something the nutrition professional can act upon directly (or influence significantly).
The purpose of identifying nutrition problems
When you identify a nutrition diagnosis, you are clarifying what needs to change, why, and how you will measure it. This gives the subsequent steps—intervention, monitoring, evaluation—direction. It helps ensure the plan is targeted, measurable, and relevant. It also enhances documentation, supports interprofessional communication, and allows for research and outcomes measurement.
Standardized Language in Nutrition: The Role of AND and NCPT
Who are the players?
Academy of Nutrition and Dietetics (AND) is the major US professional organization for dietitians. The terminology we use for the NCP is called the Nutrition Care Process Terminology (NCPT).
Why standardized language matters
Standardization means that everyone is using the same terms in the same way. This results in:
- Clearer documentation and communication between practitioners.
- Better integration into electronic health record (EHR) systems, which rely on codes and terms to function.
- Enhanced ability to conduct research, measure outcomes, aggregate data across patients, facilities and populations.
- Improved patient outcomes simply because everyone understands the problem in the same way.
How NCPT improves accuracy, research, and outcomes
The NCPT provides defined terms, arranged in a hierarchy, with unique identifiers and definitions. For example, it clearly distinguishes intake-related diagnoses (e.g., “Inadequate energy intake”), clinical diagnoses (e.g., “Impaired nutrient utilization”), and behavioral/environmental ones (e.g., “Undesirable food choices”).
This kind of structure makes it possible to map nutrition problems to broader healthcare terminologies—like SNOMED CT—so nutrition data is integrated into wider health informatics.
This means when you document in a hospital or clinic, your nutrition terminology is not floating in isolation—it can link to other disciplines, show outcomes, and support quality improvement.
The Structure of a Nutrition Diagnosis Statement
At the heart of a clear nutrition diagnosis is what’s called a PES statement. That stands for Problem, Etiology, Signs/Symptoms.
How to write an effective PES statement
- Problem (P): This is the nutrition diagnosis term itself. For example: Inadequate protein-energy intake.
- Etiology (E): The cause or contributing risk factor you can address. Example: “related to decreased food intake due to poor appetite and early satiety”.
- Signs/Symptoms (S): The evidence you found in assessment. Example: “as evidenced by 10% unintentional weight loss in last six months and serum albumin 2.8 g/dL”.
Structure:
Examples of well-written PES statements
- “Excessive carbohydrate intake related to frequent consumption of sugar-sweetened beverages as evidenced by 50 % of daily energy intake from simple sugars and HbA1c of 8.2 %.”
- “Food-and-nutrition-related knowledge deficit related to lack of access to nutrition education as evidenced by client stating ‘I don’t know how many servings of vegetables I should eat each day’ and diet recall showing < 1 serving/day of vegetables.”
These examples show how the problem, cause, and proof pieces come together. A strong PES statement makes the path forward (intervention) clearer.
Categories of Nutrition Diagnoses
The NCPT organizes nutrition diagnoses into broad categories (domains) and subcategories.
Intake-related nutrition problems
These refer to problems with food, nutrient, fluid or bioactive substance intake. Examples: inadequate energy intake, excessive fluid intake, limited food acceptance.
Clinical nutrition problems
These refer to nutrition problems related to medical or physical conditions: functionality, biochemical/weight changes, etc. For example: impaired nutrient utilization, unintentional weight loss, swallowing difficulty.
Behavioral and environmental nutrition problems
These refer to problems in behavior, knowledge, beliefs, food access, environment. For example: knowledge deficit, undesirable food choices, limited access to food or water.
Commonly Used Nutrition Diagnosis Terms
Here are some frequently encountered terms and how to think about them.
- Inadequate energy intake – When the energy (kcal) consumed is lower than what is needed.
- Unintended weight loss – A clinical category reflecting weight decline not planned or desired.
- Impaired nutrient utilization – A clinical problem where metabolism or use of nutrients is disrupted (e.g., due to disease, drug interaction).
- Food-and-nutrition-related knowledge deficit – A behavioral/environmental diagnosis when a client lacks understanding of nutrition concepts.
- Undesirable food choices – A behavioral/environmental term when the diet frequently includes foods inconsistent with health goals.
How to select the most appropriate term
- Review your assessment data: what is the problem? Are you looking at intake, clinical, or behavior/environment?
- Be as specific as possible: avoid generic terms (“poor diet”) when a defined NCPT code exists (“Undesirable food choices”).
- Ensure the term aligns with the intervention you can deliver. If you pick a term you cannot influence, it may not serve the process.
- Consider the etiology and signs/symptoms—these help guide your choice of term and how to structure your PES statement.
Differentiating Nutrition Diagnosis from Assessment and Intervention
The distinction between identifying a problem and treating it
- Assessment: Collects and analyzes data (e.g., dietary intake, labs, weight history).
- Diagnosis: Identifies a specific nutrition problem (e.g., “Inadequate protein-energy intake”).
- Intervention: What you will do about it (e.g., arrange high-protein supplement, monitor intake).
Using correct terminology ensures you don’t skip steps or blur roles—for example, you might identify inadequate intake (diagnosis), but intervention might be to provide nutrition education or adjust meal plan.
How incorrect terminology affects care plans
If you document “poor diet” instead of “Undesirable food choices related to frequent sugar-sweetened beverage consumption as evidenced by 60 % daily energy from sugar”, you risk vague intervention, unclear outcome measures, and difficulty demonstrating improvement.
Case examples highlighting these differences
- A patient’s dietary recall shows ~900 kcal/day when estimated needs are 1,800 kcal/day → Assessment data. A suitable diagnosis: “Inadequate energy intake related to limited food budget as evidenced by 30% weight loss in 3 mo.” Intervention: meal-planning education, linking to community food resources.
- A patient has BMI 34, no weight loss, eats high‐fat fast food most days → Assessment: dietary pattern, weight status. Diagnosis: “Overweight/obesity related to frequent fast-food consumption and minimal home-cooked meals as evidenced by BMI 34 kg/m² and 5 meals/week fast food.” Intervention: behavior-change counselling, goal-setting, home cooking initiative.
Tools and Resources for Learning Nutrition Diagnosis Terminology
- The NCPT is available electronically via eNCPT (an online subscription managed by the Academy).
- The NCPT Reference Manual (print/ebook) is available for dietitians who want the full list of terms, definitions, etiology matrices, etc.
- Free terms lists: e.g., the “Freely Available NCP Terms” list offers commonly used terms and definitions.
- Continuing education, webinars, university coursework in dietetics all often include modules on the NCP and NCPT.
- For documentation and EHR integration: hospital systems may offer training on how to map NCPT diagnoses to clinical workflows.
If you’re studying or practicing in dietetics, it’s wise to become familiar with the major domains, how to construct PES statements, and where to look up terms when you’re unsure.
Practical Application in Clinical Settings
How dietitians use nutrition diagnosis terminology in hospitals, clinics, and community programs
In a hospital setting, a registered dietitian may assess a patient, identify “Swallowing difficulty” (clinical domain) as a nutrition diagnosis, and then implement intervention (e.g., referral to speech therapist, texture-modified diet). Using correct terminology ensures the medical record reflects the nutrition professional’s role.
In community programs, you might identify “Limited access to food or water” (behavioral/environmental domain) for a low-income client—then plan intervention to connect them with food assistance. The terminology helps you clearly document the barrier you’re addressing.
Integration into electronic health records (EHRs)
Thanks to the NCPT being increasingly mapped to healthcare terminology systems such as SNOMED CT, nutrition diagnoses can be encoded in EHRs and used for data analytics, outcome tracking, interdisciplinary communication.
Case study examples
Case A (Hospital): A 67-year-old male post-cardiac surgery, poor appetite, 12% weight loss over 2 months. Nutrition diagnosis: “Unintended weight loss related to inadequate energy intake as evidenced by 12% weight loss over 2 months and reported intake of 700 kcal/day.” Intervention: high-energy, high-protein diet, oral nutrition supplement, monitor weight weekly.
Case B (Community): A 45-year-old female managing type 2 diabetes, eats > 5 sugar-sweetened beverages/day, HbA1c 9.1%. Nutrition diagnosis: “Excessive carbohydrate intake related to frequent consumption of sugar-sweetened beverages as evidenced by > 5 servings/day sugar-sweetened beverages and HbA1c 9.1%.” Intervention: beverage substitution plan, client education, weekly follow-up.
These examples show how using precise terminology clarifies the problem, cause and evidence—and sets up the intervention and monitoring in a logical way.
Challenges in Applying Nutrition Diagnosis Terminology
Common mistakes when formulating diagnoses
- Using vague language: “Poor diet” or “Needs improvement” instead of a defined NCPT term like “Undesirable food choices”.
- Writing a statement that lacks clear etiology or signs/symptoms: e.g., “Inadequate nutrient intake” without specifying cause or evidence.
- Selecting a diagnosis outside the practitioner’s scope (i.e., not actionable).
Limitations of current terminology
Although NCPT is robust, some limitations exist:
- Some settings may lack terminology translations or local adaptations (especially outside the U.S.).
- Some EHR systems may not be fully integrated with NCPT, making documentation cumbersome.
- The granularity of terms may sometimes overwhelm users—too many options can lead to confusion.
Overcoming barriers to proper usage
- Training and continuous professional development to become fluent in terminology.
- Use “reference sheets” (provided by NCPT) to guide term selection, supporting evidence, and measurement indicators.
- Engage with informatics/IT teams so EHR workflows align with nutrition terminology.
- Foster peer review and feedback in your workplace: regular discussion about correct PES statements, documentation standards.
- Advocate within your institution for nutrition documentation standards and integration.
The Importance of Consistency and Accuracy
Why does it matter so much that terminology is both consistent and accurate? Because the ripple effects are real.
For patient outcomes
When the nutrition diagnosis is clearly defined and targeted, the resulting intervention is more likely to be appropriate and effective. Conversely, a fuzzy diagnosis can lead to vague interventions and poor tracking of outcomes.
For interprofessional communication
Nutrition professionals are rarely working in isolation. Physicians, nurses, pharmacists, therapists—all rely on clear documentation. When you state “Impaired nutrient utilization related to medication–nutrient interaction as evidenced by lab X,” everyone understands the nutrition issue, its cause, and how it links to medical care.
Examples of miscommunication due to vague language
Imagine a dietitian writes “Poor appetite” but does not tie it to intake or weight changes—and the physician interprets it differently than the dietitian. The intervention might be delayed or mis-directed. In contrast, a clear statement like “Inadequate energy intake related to poor appetite as evidenced by 15% weight loss in 3 months and intake < 800 kcal/day” leaves little ambiguity.
In sum: consistent accurate terminology supports continuity of care, measurable outcomes, research, quality improvement—and ultimately better patient results.
Future Developments in Nutrition Diagnosis Terminology
Emerging trends in nutrition informatics
Terminology is increasingly integrated with digital health tools, EHRs, dashboards, analytics for nutrition outcomes. For example, linking nutrition diagnosis data to cost of care, length of stay, disease outcomes.
Digital tools improving standardized language use
Platforms like eNCPT make it easier to search, map, document nutrition terms. There are also tutorials, case studies and reference materials that train dietitians in the use of standardized terminology.
Expected updates in NCPT terminology
The NCPT is actively maintained and updated. For example, an editorial guidance document cites how new terms are reviewed, approved, mapped to standard health terminologies. Also, in 2024 the inclusion of NCPT into SNOMED CT reference set highlighted the evolution of nutrition terminology at a global level.
Future updates will likely bring more granularity, global applicability, mapping to international EHR systems, and perhaps greater use in population-health and preventative nutrition.
As technology and health data evolve, the expectation is that nutrition care—and its language—will become ever more integrated into the broader health system. For dietitians and nutrition professionals this means staying current is vital.
Case Studies: Real-World Examples
Example 1: Malnutrition diagnosis
A 78-year-old woman admitted to a rehabilitation unit after hip surgery. Assessment: 14% unintended weight loss in 4 months, BMI 17.5 kg/m², reduced muscle mass on physical exam. Intake is low (<750 kcal/day).
PES statement: “Malnutrition (undernutrition) related to inadequate energy-protein intake due to decreased appetite and impaired mobility as evidenced by 14% weight loss in 4 months, BMI 17.5 kg/m² and reported intake < 750 kcal/day.”
Using this label guided the nutrition intervention (high‐energy, high‐protein diet, nutrition support, mobility assistance) and monitoring of weight, intake, muscle strength.
Example 2: Inadequate protein-energy intake
A 54-year-old male with chronic kidney disease (stage 3), reports eating mostly convenience foods, protein intake ~0.6 g/kg/day (target 0.8 g/kg/day). He has mild edema and low albumin.
PES statement: “Inadequate protein-energy intake related to frequent use of convenience foods rather than meals as evidenced by protein intake 0.6 g/kg/day, serum albumin 3.1 g/dL and mild lower-extremity edema.”
This pinpointed the nutrition problem, grounded it, and enabled measurable goals (increase protein to 0.8 g/kg/day, get albumin above 3.5 g/dL, reduce edema).
Example 3: Disordered eating behavior
A 30-year-old female, recently diagnosed with polycystic ovary syndrome (PCOS), reports frequent binge-eating episodes triggered by stress and negative body image. Weight has steadily increased by 8% in one year, and fasting insulin is elevated.
PES statement: “Disordered eating pattern related to emotional eating during stress and negative body image as evidenced by self-reported 3 binge-eating episodes/week, 8% weight gain in 12 months and fasting insulin > 25 µU/mL.”
By using this terminology, the dietitian can document a behavioral-environmental domain diagnosis, plan appropriate behavioral intervention (stress-management, structured meal plan, referral to counselor) and monitor episodes and weight changes.
These real-world examples show how using precise, standardized nutrition diagnosis terminology impacts how care is delivered, documented, and measured.
Conclusion and Key Takeaways
In short: mastering nutrition diagnosis terminology is not just an administrative exercise—it’s foundational to effective nutrition care. When you work with precise, standardized terms, framed in a clear PES statement, you clarify the problem, root cause and measurable evidence. This sets up the entire care plan to be focused, measurable and relevant.
Here are the key takeaways:
- A nutrition diagnosis is a specific problem within your scope of practice—it is not the same as a medical diagnosis.
- The NCP framework (Assessment → Diagnosis → Intervention → Monitoring/Evaluation) gives structure to nutrition care, and terminology is central in the Diagnosis step.
- Using the NCPT (via the Academy of Nutrition and Dietetics) ensures you and your colleagues are speaking the same language, which improves communication, documentation, research and outcomes.
- The PES statement (Problem / Etiology / Signs–Symptoms) is the format that links diagnosis to its cause and its proof—getting it right matters.
- Knowing the categories of nutrition diagnoses (intake, clinical, behavioral/environmental) and familiarizing yourself with common terms improves your precision.
- Documentation that uses vague language weakens the intervention and makes evaluation difficult. Accurate, consistent terminology strengthens your care plan and outcomes.
- The field is evolving: digital tools, informatics, broader health-system integration—and staying current is essential.
If you are a dietitian, nutrition professional, student or educator, I encourage you to dig into the NCPT terms, practice writing PES statements, review case studies, and discuss with peers or mentors. Consistency in terminology makes real difference—not just for documentation, but for the clients you serve.
Finally: think of the terminology as your professional toolset. A sharp toolset makes the job smoother, clearer and more effective. Use it well—and your nutrition care will reflect that clarity.